Basic Understanding of Diabetes
A list of frequently asked questions to help you understand how it works.
What are the symptoms of diabetes mellitus?
Both Type 1 and type 2 diabetes can lead to following symptoms:
- Needing to urinate often/ especially at night
- Intense thirst
- Blurry vision
- Increased hunger
- Delayed wound healing
- Fungal infections especially in the skin
Type 1 Diabetes can present with diabetic ketoacidosis where high sugars are associated with abdominal pain, nausea and vomiting, abdominal pain, shortness of breath, fruity-scented breath, confusion and above symptoms.
Type 2 diabetes usually causes no symptoms in many patients.
What is type 2 diabetes?
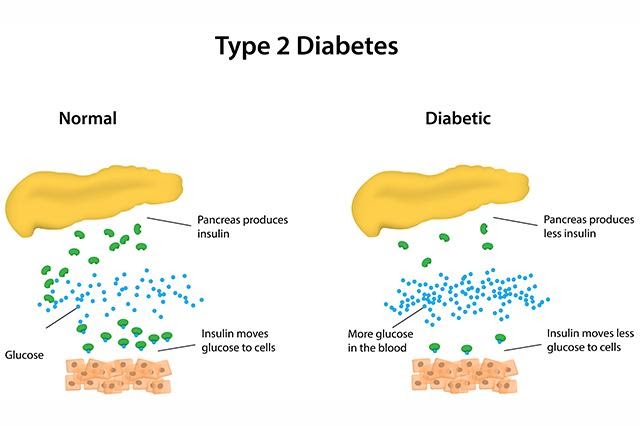
Type 2 diabetes mellitus is a disorder that disturbs the way your body uses/metabolises sugar.
All the cells in your body need sugar to work normally. It’s the basic fuel of the body. Sugar gets into the cells with the help of a hormone called insulin.
If there is decreased insulin, or if the body stops responding to insulin, sugar increases in the blood. That is what happens to people with diabetes.
There are 2 different types of diabetes. In type 1 diabetes, the problem is that the body makes little or no insulin.
In type 2 diabetes, the problem is that:
- The body’s cells do not respond to insulin aka “INSULIN RESISTANCE”
- The body does not make enough insulin
- Or both
If type 2 diabetes rarely causes symptoms, why should I care about it?
Even though type 2 diabetes might not cause symptoms, it can still cause serious problems over time, if it is not treated. It can lead to following complications:
- Heart attacks
- Strokes
- Kidney failure
- Vision problems or even blindness
- Pain or loss of sensations in the hands and feet
- Foot ulcers and gangrenes
Can type 2 diabetes be prevented?
Yes, it can. To reduce your chances of getting type 2 diabetes, the most important thing you can do is control your weight. If you already have the disorder, losing weight can improve your health and blood sugar control. Being active can also help prevent or control the disorder.
Can diabetes be genetic?
The cause of type 2 diabetes is a complex interplay of genetic, lifestyle factors, some of which have not been identified. Studies have identified at least 150 DNA variations that are associated with the risk of developing type 2 diabetes These genes are involved in many aspects of type 2 diabetes, including the development and function of beta cells in the pancreas, the release and processing of insulin, and cells' sensitivity to the effects of insulin.
Most of these changes are common and are present both in people with diabetes and in those without. Each person has some variations that increase risk and others that reduce risk. It is the combination of these changes that helps determine a person’s likelihood of developing the disease. Thus Type 2 diabetes is caused by both genetic and environmental factors and it can be difficult to separate genetic risk from environmental risk.
If you have family history of diabetes is it true that you have a high probability of getting it as well? If so why?
Family studies have revealed that first degree relatives of individuals with Type 2 Diabetes are about 3 times more likely to develop the disease than individuals without a positive family history of the disease. However, that doesn’t mean that if your mother or father has (or had) type 2 diabetes, you’re guaranteed to develop it; instead, it means that you have a greater chance of developing type 2. As discussed earlier your genes inherited from parents make you more prone however the environmental factors like healthy eating habits, exercise etc. also are likely to pass on to the next generation as shared behaviour which increases the risk of developing type 2 diabetes.
How do you prevent diabetes if you have a strong family history?
Making lifestyle adjustment to diet and physical activity is the key to prevent diabetes. Keep your weight and BMI in control as per Indian standards. Check you sugars i.e. Fasting plasma glucose and Glycated hemoglobin (Hba1c) at least once a year over if not in ideal BMI range.