How is blood sugar testing done ?
If you have diabetes, you have an important role in your own medical care and monitoring your blood sugar (glucose) level is a key part of this.
The main goal of diabetes treatment is to keep your blood sugar levels in the target range. Checking your blood sugar is one of the best ways to know how well your diabetes treatment plan is working.
Blood sugar can be tested with:
- Laboratory checking of fasting and post lunch sugars
- Glycated haemoglobin (HbA1C): The A1C test gives an overall sense of how blood sugar levels are controlled since it measures your average blood sugar level of the past two to three months
- Fingerstick blood glucose meter also known as SMBG (Self-Monitoring of blood glucose levels)
- Continuous glucose monitoring (CGM) device.
How to check your blood sugar with a Glucose Meter (glucometer) ?
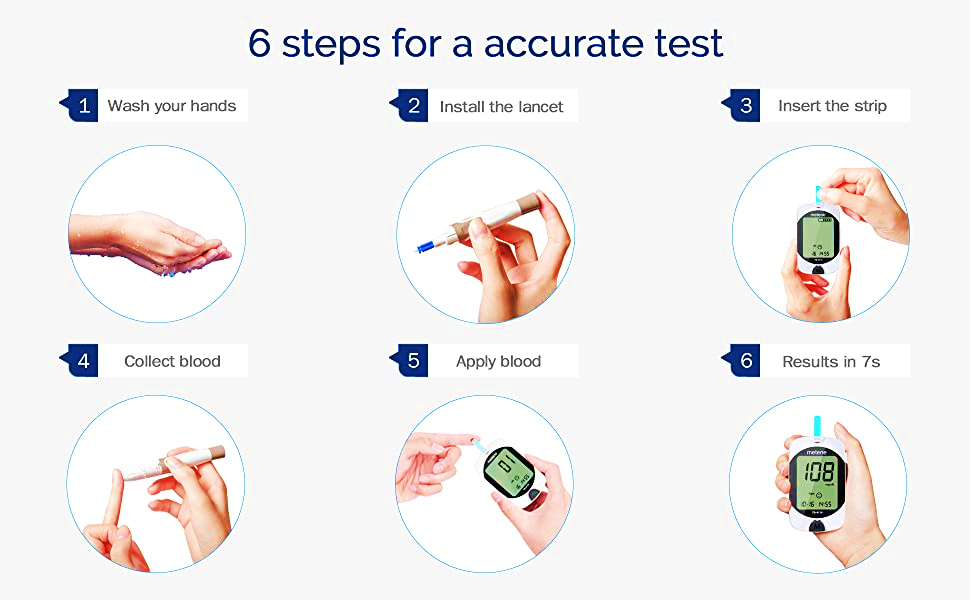
The following steps include general guidelines for testing blood sugar levels. However, because the instructions can vary between devices, it’s best to check the package insert for your glucose meter or talk with your health care provider. It’s important to never share monitoring equipment or fingerstick devices, as this could lead to infection.
- Wash hands with soap and warm water, then dry.
- Prepare the lancing device by inserting a fresh lancet. Lancets that are used more than once are not as sharp as a new lancet and can cause more pain and injury to the skin.
- Prepare the blood glucose meter and test strip (the exact instructions for this depend upon the type of glucose meter used).
- Use the lancing device to obtain a small drop of blood from your fingertip or alternate site (like the skin of the forearm). Alternate sites are often less painful than the fingertip. However, results from alternate sites are not as accurate as fingertip samples. This should not be a problem if you always use the same site.
However, when your blood sugar is rising rapidly (eg, immediately after eating) or falling rapidly (in response to insulin or exercise), it’s more accurate to use the fingertip, as testing at alternate sites may give significantly different results in these situations.
If you have difficulty getting a good drop of blood from your fingertip, try rinsing your fingers with warm water and shaking your hand below your waist. This can help get the blood flowing.
- Apply the blood drop to the test strip in the blood glucose meter. The results will be displayed on the meter after several seconds.
- Dispose of the used lancet in a container designed for sharps (not in household trash).
How frequent should I test my BLOOD SUGAR Levels?
How often you need to check your blood sugar will depend upon the type of diabetes you have (type 1 or 2), which treatment(s) you use (oral medications, insulin, and/or lifestyle changes), and your treatment goals.
Type 1 diabetes —
For people with type 1 diabetes, frequent testing with glucose meters (SMBG) is the only way to safely and effectively manage blood sugar levels. Most people need to test at least four times per day. If you use an insulin pump, give yourself three or more insulin injections per day. HbA1c is usually done 3 monthly.
Type 2 diabetes —
For people with type 2 diabetes, the recommendations for how often to test blood sugar are based upon individual factors such as type of treatment (oral medications, insulin, and/or lifestyle changes), A1C level, risk of hypoglycaemia (when blood sugar is too low), and treatment goals.
Blood sugar monitoring is useful for people with type 2 diabetes who take insulin or certain medications that can cause hypoglycaemia. It is generally unnecessary in people who manage their diabetes with diet alone or who take medications that do not cause hypoglycaemia. Your doctor will help you determine how frequently to check your blood sugar based on your situation.
What Blood glucose meter should I use?
There is no single blood glucose meter that is better than others.
Your doctor can help you choose a meter based on your preferences as well as other factors like cost, ease of use, and accuracy; it should be one that is approved by either the International Organization for Standardization or the US Food and Drug Administration.
How accurate are blood glucose monitoring machines?
- Blood glucose meters are reasonably accurate. However, there can be some variability between meters, so it is always wise to use caution and common sense.
- If you get a result that does not fit with how you feel (for example, if it says your blood sugar is very low but you don’t have any symptoms), take a second reading or use an alternate method for testing your blood sugar (such as a different meter). Blood glucose meters are least accurate during episodes of low blood sugar.
- The accuracy of blood glucose monitoring can be affected by several factors, including the type of blood glucose strip and meter. It’s a good idea to check the accuracy of your blood glucose meter occasionally by bringing it with you when you have an appointment to get blood testing.
This way, you use your home monitor to check your blood sugar while blood is drawn and compare the results. If the results differ by more than 15 percent, there may be a problem with your meter or other equipment; your provider can help you figure out what’s going on and how to correct the problem.
What is a CONTINUOUS GLUCOSE MONITORING SYSTEM?
- Continuous glucose monitoring (CGM) is a way to monitor your blood sugar levels every 5 to 15 minutes, 24 hours a day. Because of reliability issues and the need to calibrate some of the devices, CGM does not eliminate the need for at least occasional fingerstick.
- CGM systems use a glucose sensor to measure the level of glucose in the fluid under the skin. The sensor is attached to a transmitter placed on your skin, which is held in place with a sticky patch. It wirelessly transmits results to a small recording device (no larger than a cell phone) or to a smartphone or other smart device. In some cases, it transmits the information directly to an insulin pump. You can attach the recording device to your clothing, carry in a purse or bag, or place it near you (eg, on a bedside table).
- If you use a CGM system, you will need to remove the sensor and replace it on a different part of your body approximately once every 7 to 14 days. Different CGM systems are available.
Who should use the CGM systems?
CGM systems are most often used by :
- People with type 1 diabetes who give themselves multiple daily insulin injections or use an insulin pump.
- People who have frequent episodes of low blood sugar, episodes of low blood sugar during the night (“nocturnal hypoglycemia”), large fluctuations in their blood sugar levels, and/or difficulty recognizing when they have low blood sugar.
- Intermittent use for some people with type 2 diabetes who need multiple daily insulin injections, particularly those with frequent episodes of low blood sugar or difficulty recognizing when they have low blood sugar.
- Sometimes in pregnancy especially with type 1 Diabetes
